IV INSERTION TECHNIQUES UPDATED – NURSING PROCEDURES AND SKILLS
IV INSERTION TECHNIQUES – NURSING PROCEDURES AND SKILLS
Intravenous (IV) insertion is a critical skill for nurses and healthcare professionals, used to administer medications, fluids, and other therapies directly into a patient’s bloodstream. Proper IV insertion technique requires both technical skill and knowledge of anatomy. Below is a detailed overview of IV insertion techniques and skills.
1. Preparation for IV Insertion
- Assess Patient:
- Check the patient’s medical history, current condition, and any previous IV insertion issues (e.g., difficult veins, allergies to adhesives, etc.).
- Consider the appropriate vein for IV insertion based on patient factors like dehydration, obesity, or edema.
- Educate the patient about the procedure to reduce anxiety and gain consent.
- Gather Equipment:
- IV catheter (choose the appropriate gauge; 18G–24G depending on patient size and purpose of IV).
- IV start kit (includes tourniquet, antiseptic wipes, sterile gauze, adhesive tape or securement device).
- Saline flush, extension tubing, or IV fluids if required.
- Gloves and any required PPE (Personal Protective Equipment).
- Sharps disposal container for used needles.
- Hand Hygiene and PPE:
- Perform hand hygiene (wash hands or use an alcohol-based sanitizer) and don gloves to prevent infection.
2. Selecting the Vein
- Common IV Sites:
- Dorsal hand veins: Suitable for short-term therapy and smaller gauges.
- Forearm veins (cephalic, basilic veins): Common site for IV insertion, offering good mobility.
- Antecubital fossa veins: Used for larger catheters or in emergency situations.
- Vein Characteristics:
- Choose veins that are palpable, soft, and have a straight path. Avoid areas with scarring, bruising, or signs of infection.
- Avoid inserting into veins near joints as patient movement may dislodge the catheter.
3. IV Insertion Technique
- Apply Tourniquet:
- Place the tourniquet around the upper arm (about 3–4 inches above the insertion site). Ensure it is tight enough to obstruct venous flow but not arterial flow, making veins more prominent.
- Palpate and Identify Vein:
- Palpate the vein to ensure it is well-filled, soft, and straight. Avoid veins that are too small, hard, or tortuous.
- Disinfect the Site:
- Clean the insertion site with an antiseptic wipe (usually chlorhexidine or alcohol) in a circular motion, starting at the center and moving outward. Allow the area to dry completely to prevent irritation.
- Hold the Skin Taut:
- With your non-dominant hand, hold the skin taut below the insertion site to stabilize the vein and minimize movement.
- Insert the Needle:
- Hold the catheter in your dominant hand at a 15–30 degree angle with the bevel of the needle facing up.
- Insert the needle into the vein in a smooth, steady motion. Once you feel a “pop” or see a flash of blood in the flashback chamber, lower the angle of insertion and advance the needle slightly.
- Advance the Catheter:
- After confirming venous access (blood flashback), advance the catheter into the vein while holding the needle steady. Ensure the catheter is fully inserted and the needle is withdrawn safely.
- Release the Tourniquet:
- Release the tourniquet as soon as the catheter is in place to restore venous flow and prevent backflow.
- Secure the Catheter:
- Attach the extension set or IV tubing to the catheter hub. Flush the catheter with saline to confirm patency (check for swelling or discomfort).
- Secure the catheter with adhesive tape, a securement device, or a transparent dressing to keep the IV in place and prevent dislodgement.
- Dispose of Needle Safely:
- Immediately place the used needle into a sharps container to prevent accidental needlestick injuries.
4. Post-Insertion Care
- Monitor for Complications:
- Observe the site for signs of infiltration (swelling, coolness), phlebitis (redness, warmth, tenderness), or infection.
- Ensure the IV is functioning correctly by checking for adequate flow and monitoring the patient’s response.
- Document the Procedure:
- Document the time of insertion, gauge of the catheter, location of the insertion, number of attempts, and any patient responses or complications.
- Check for Proper Flow:
- Ensure the IV is infusing at the correct rate by monitoring the flow of fluids or medication. If using an IV pump, verify the settings.
5. Techniques for Difficult IV Access
- Warming the Site: Applying a warm compress can help dilate veins and make them more visible, especially in patients with poor peripheral circulation.
- Vein Visualization: Use vein visualization devices or ultrasound guidance to locate difficult veins, particularly in obese or pediatric patients.
- Hydration: Ensure the patient is well-hydrated, as dehydration can make veins more difficult to locate and access.
- Tourniquet Positioning: For difficult veins, consider using a blood pressure cuff instead of a tourniquet to gently constrict veins.
6. Complications and Troubleshooting
- Infiltration: Occurs when IV fluid leaks into surrounding tissue. Signs include swelling, coolness, and pain at the site. If infiltration occurs, remove the IV and restart it in a different location.
- Phlebitis: Inflammation of the vein, often due to irritation from the catheter. Look for redness, warmth, and tenderness along the vein. Remove the IV and consider switching to a smaller gauge or different vein.
- Air Embolism: Ensure no air is introduced into the IV line, as air embolism can be life-threatening. Use saline flushes and inspect IV tubing for air bubbles.
- Hematoma: Occurs if the vein is punctured and blood leaks into surrounding tissue. To prevent this, apply pressure after removing the IV and avoid excessive probing with the needle.
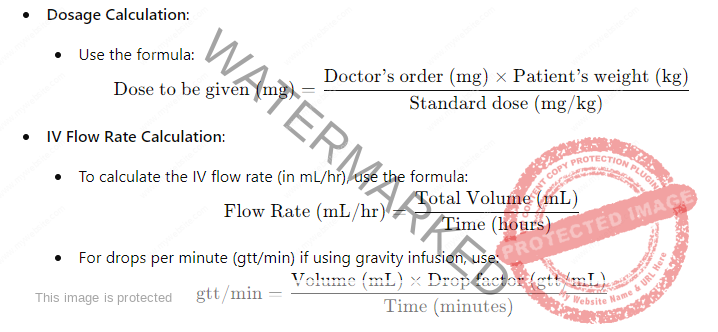
7. Dosage Calculation and IV Rate Calculation
8. IV Skill Proficiency
- Practice and Competence: Regular practice in IV insertion improves proficiency. Nurses should be comfortable with varying IV sites, gauges, and patient types (e.g., pediatrics, geriatrics, critically ill).
- Staying Updated: IV insertion techniques evolve with new devices and infection prevention protocols, so staying updated on best practices is essential for all healthcare providers.
By mastering these techniques and skills, healthcare professionals can ensure safe, efficient, and effective IV insertion and management for their patients.
