TYPES AND CARE OF
HEALTH RECORDS –
A SIMPLE NURSING GUIDE
Effective communications among health professionals is essential for the coordination and continuity of care. Documentation (Health Records) is the written, legal record of all pertinent interactions with the client – assessing, diagnosing, planning, implementing and evaluating.
Record keeping systems are either handwritten or computerized and the format varies among health care agencies. Nowadays, sophisticated management information system is utilized to manage client specific data and information. These records are used to facilitate client care, serve as financial and legal records, help in clinical research and support decision analysis.
Health records are the compilation of a client’s health information. The patient’s health record is a brief account of personal and medical history of the client, results of diagnostic test, findings of medical examination, treatment and nursing care, daily progress notes and advice on discharge. Each health care institution has policies that specify the nurse’s documentation responsibilities.
CARE OF HEALTH RECORDS
1. The records are kept under the safe custody of the nurse in each ward or department.
2. No individual sheet is separated from the complete record.
3. Records are kept in a place, not accessible to the clients and visitors.
4. No stranger is ever permitted to read the records.
5. Records are not handled over to the legal advisors without the written permission of the administration.
6. All hospital personnel are legally and ethically obligated to keep in confidence all the information’s provided in the records.
7. All records are to be handled carefully. Careless handling can destroy the records.
8. All records are filed according to the hospital custom so that they can be traced easily. Records could be arranged:
a. Alphabetically
b. Numerically
c. With index cards
d. Geographically
All records are identified with the bio data of the clients such as name, age, ward, bed no., O.P. no., diagnosis etc.
Records are never sent out of the hospital without the doctor’s permission. Reference is made by writing separate sheets and sending to the agency who requests for them e.g., reference letters, discharge summaries.
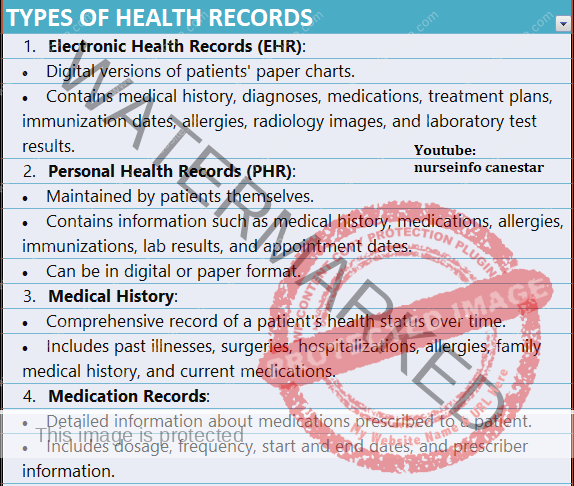
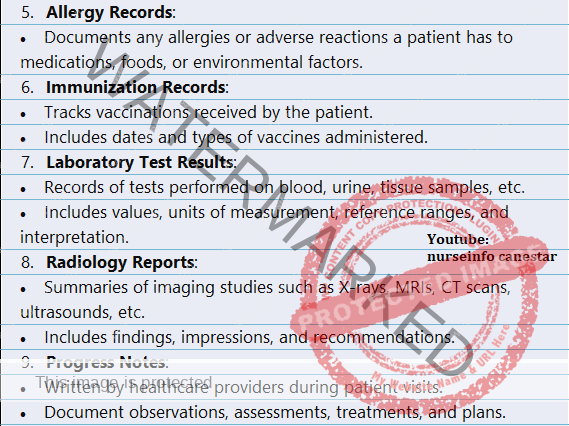
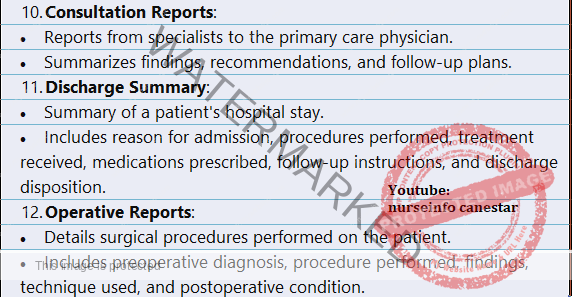
TYPES OF HEALTH RECORDS
1. Outpatient and Inpatient Records
In most of the hospitals, the inpatient record will be continuation of the outpatient record. Outpatient record is filled up in the outpatient department. This will contain the bio data of the client, diagnosis, family history, history of the past and present illness, signs and symptoms, findings of medical examination, investigations, treatments, medications, progress notes and summary made at the discharge of the client.
2. Nurse’s recording
Large part of the client’s records is filled by the nurses. Nurse’s notes are a record of treatments and nursing measures carried out by the nurses, their effects, the observations made on the client. Avoid bulky reports containing unnecessary and irrelevant materials.
Observation of the client is continuous and it is impossible for the nurse to record all her observations. She should record what she thinks that might affect the diagnosis, medical treatment, nursing care and rehabilitation. Observation should be as specific and objective as possible. The following points will serve as a guide in selecting the important symptoms.
a. Symptoms that are intense or severe in character, e.g., a colicky pain.
b. That persists over a long period.
c. That indicates a change in the condition of the client.
d. That indicates an impairment or loss of function of an organ or a part of the body.
e. That recurs at regular or stated intervals.
f. That becomes progressively more severe.
g. That may indicate development of complications.
h. That requires treatment beyond the ordinary nursing measures.
3. Doctor’s Order Sheet
The doctor’s orders (prescriptions) regarding the medication investigations, diet etc., may be written on separate sheets.
4. Graphic Charts of T.P.R.
On this the temperature, pulse and respirations are written in a graphic form so that a slight variation from the normal can be noted at a glance.
Other information such as blood pressure, number of bowel movements, the body weight, name and date of operation, removal of sutures etc. may be recorded on this chart according to the hospital customs
5. Reports of Laboratory Examinations
6. Diet Sheets
7. Consent Form for Operations and Anaesthesia
8. Intake and Output Chart
Client on intravenous fluids or on the fluid diet, critically ill clients, post-operative clients, clients with oedema, clients having vomiting and diarrhea, clients getting diuretics etc., should have their intake and output maintained.
9. Reports of Anaesthesia, Physiotherapy, Occupational Therapy and Other Special Treatments.
10. Registers
To maintain the statistics, every hospital maintains certain registers such as registers for the births and deaths, registers for operations and deliveries, census register, register for the admission and discharges, register for the O.P.D. attendants etc. it is the nurse’ s responsibility to maintain these registers up to date.
Medicolegal Cases – Record
The important documents to be maintained by the hospital in MLC and RTA cases are as follows:
a. Police intimation: this has to be given to the nearest police station by the hospital.
b. Wound Certificate: these are given on request by the police. It must be duly signed by the medical officer, who has attended the client.
c. Discharge certificate: this is given on demand from the police for MLC and RTA cases.
d. Accident cum wound register: this is usually maintained by the casualty medical officer. In case the client demands, medical certificate may have to be issued by the hospital.
Medication Record
It consists of designated areas to record name and dose of drug, date and time of administration, route and frequency of administration and the nurse’s signature. Some records also allow documenting any drug allergy.
Daily Nursing Care Record
This includes diet, hygiene, elimination, treatment, diagnostic studies etc.
Nursing Discharge/Referral Summaries
This is made on discharge of a client or at the time of transfer of a client to another health care institution.
Long-Term Care Documentation
This depends on the policy and standard of the health agency.
Home Care Documentation
In this, two records are usually utilized.
1. A home health certification and plan of treatment form.
2. A medical update and client information.
Kardexes
The kardex is widely used. It is a concise method of organizing and recording data about a client, making information quickly accessible to all health professionals. The system consists of series of cards kept in a portable index file. Particular client’s card can be quickly traced in case any need arises.
Flowsheets
These are otherwise called abbreviated progress notes which give a quick and clear picture of the client’s condition.