Medical and Nursing Cheat Sheet for Medical Professionals
A medical cheat sheet serves as a condensed reference guide, offering a snapshot of key medical facts, protocols, and guidelines. Its compact format is designed for ease of use, allowing healthcare providers to retrieve information rapidly during clinical practice, examinations, or while on the go.
This cheat sheet encompasses a range of topics relevant to everyday medical practice, including:
- Clinical Guidelines: Quick summaries of diagnostic criteria, treatment protocols, and best practices.
- Pharmacology: Common medications, dosages, contraindications, and interactions.
- Vital Signs: Normal ranges for different age groups and their clinical significance.
- Medical Terminology: Definitions of frequently used terms and acronyms.
- Emergency Procedures: Steps for handling critical situations like cardiac arrest, trauma, and respiratory distress.
Intended Use This cheat sheet is designed for medical students, residents, nurses, paramedics, and other healthcare professionals. It serves as a supplementary tool, not a replacement for detailed textbooks or medical databases. Users should always rely on their clinical judgment and institutional protocols when making decisions, using this cheat sheet as a quick refresher or reference point.
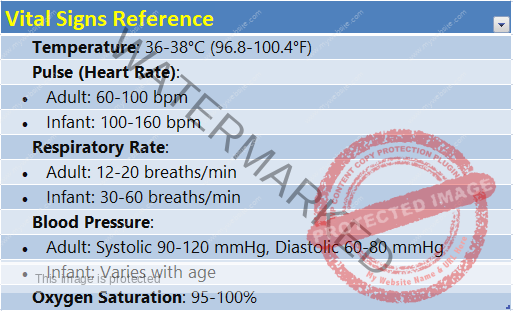
VITAL SIGNS
Vital signs are essential indicators of a person’s general health status and can provide critical information during medical assessment and ongoing monitoring.
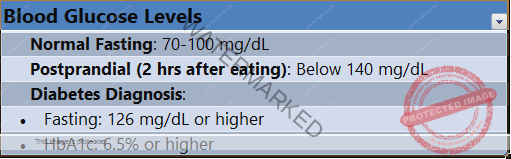
BLOOD GLUCOSE LEVELS
Blood glucose levels are an important measure of metabolic health, particularly for diagnosing and managing diabetes.
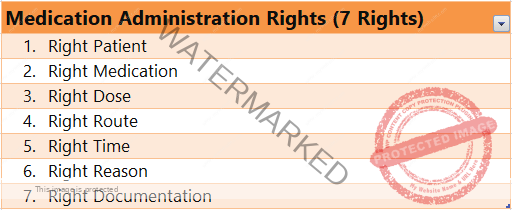
MEDICATION ADMINISTRATION RIGHTS ( 7 RIGHTS)
The “Rights” of medication administration are a set of principles designed to ensure the safe and effective delivery of medication to patients. These guidelines are foundational in reducing medication errors and ensuring patient safety.
IV FLUIDS
Intravenous (IV) fluids are liquids given to patients directly into their veins to maintain or restore fluid balance, electrolytes, and hydration. They are commonly used in hospitals, clinics, emergency settings, and surgeries. IV fluids come in various types, each with specific indications and purposes.
Types of IV Fluids
IV fluids are generally classified into three categories: crystalloids, colloids, and blood products.
1. Crystalloids
Crystalloids are solutions containing small molecules that can move easily across membranes, making them suitable for various medical purposes.
- Normal Saline (0.9% Sodium Chloride)
- Use: Hydration, volume resuscitation, flushing IV lines, and diluting medications.
- Considerations: May cause hypernatremia or hyperchloremic acidosis if used in large amounts.
- Lactated Ringer’s (Ringer’s Lactate, Hartmann’s Solution)
- Use: Volume resuscitation, electrolyte replacement.
- Considerations: Contains sodium, chloride, potassium, calcium, and lactate. Avoid in severe renal or liver disease due to potassium and lactate content.
- Dextrose in Water (D5W)
- Use: Hydration, hypoglycemia, and as a carrier for medications.
- Considerations: Rapidly metabolized, leaving free water. Can lead to hyperglycemia in large amounts or prolonged use.
- Half-Normal Saline (0.45% Sodium Chloride)
- Use: Hydration, especially in hypernatremia.
- Considerations: Potential for hyponatremia in large volumes.
2. Colloids
Colloids contain larger molecules that do not easily pass through membranes, providing oncotic pressure to maintain fluid in the vascular compartment.
- Albumin
- Use: Hypoalbuminemia, hypovolemia, and volume expansion in certain cases (e.g., liver disease, nephrotic syndrome).
- Considerations: Higher cost; potential allergic reactions; not typically first-line for routine fluid resuscitation.
- Hydroxyethyl Starch (HES)
- Use: Volume expansion in hypovolemic shock.
- Considerations: Associated with coagulopathy, kidney injury, and increased mortality; limited use in critical care.
3. Blood Products
Blood products are used to replace blood components and provide oxygen-carrying capacity.
- Packed Red Blood Cells (PRBCs)
- Use: Blood loss, anemia, and restoring oxygen-carrying capacity.
- Considerations: Requires cross-matching; risk of transfusion reactions.
- Fresh Frozen Plasma (FFP)
- Use: Coagulopathy, massive transfusions, and liver disease.
- Considerations: Requires thawing; carries transfusion-related risks.
- Platelets
- Use: Thrombocytopenia, platelet dysfunction, or bleeding.
- Considerations: Short shelf life; may cause transfusion reactions.
Indications for IV Fluids
- Volume Resuscitation: For hypovolemia due to blood loss, dehydration, or shock.
- Hydration: For patients unable to drink sufficient fluids.
- Medication Delivery: Using IV fluids to deliver medications.
- Electrolyte Replacement: To correct imbalances in sodium, potassium, etc.
- Nutritional Support: Total parenteral nutrition (TPN) for patients who cannot eat by mouth.
Considerations and Risks
- Fluid Overload: Excessive fluid administration can lead to pulmonary edema, heart failure, or other complications.
- Electrolyte Imbalances: Care must be taken to avoid hypernatremia, hyponatremia, hyperkalemia, etc.
- Compatibility: Ensure compatibility with other medications or fluids.
- Infection Risk: Proper aseptic technique and IV site monitoring are essential to prevent infections.
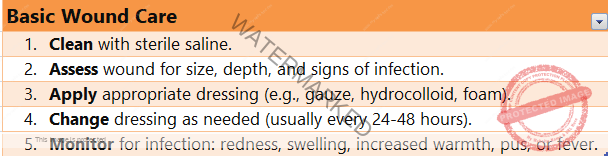
BASIC WOUND CARE
Wound care is a critical aspect of healthcare, encompassing the assessment, treatment, and management of various types of wounds. Proper wound care promotes healing, reduces the risk of infection, and prevents complications.
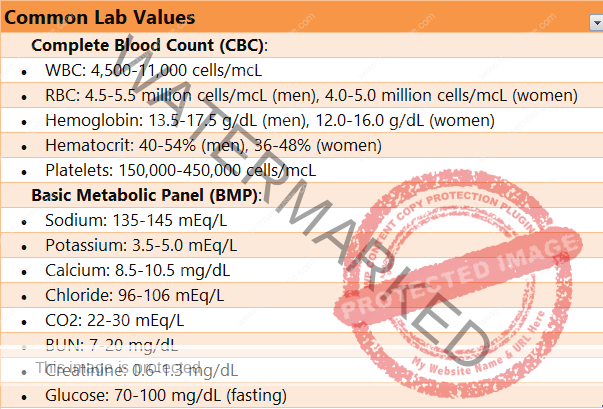
COMMON LAB VALUES
Lab values, also known as laboratory reference ranges, are the numerical ranges for various biological markers that are typically tested to assess health and diagnose diseases. Knowing these reference ranges helps healthcare professionals interpret test results and guide clinical decisions.
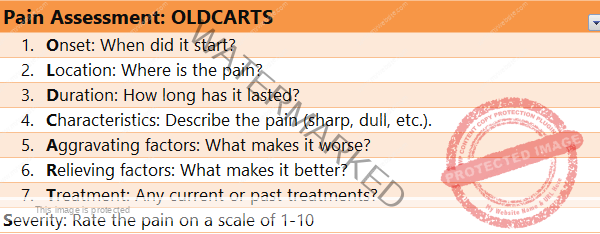
Pain Assessment: OLDCARTS
Pain assessment is a crucial component of healthcare, allowing healthcare professionals to understand the intensity, location, and quality of a patient’s pain to determine appropriate management strategies. Accurate pain assessment helps guide treatment decisions, monitor progress, and improve patient outcomes.
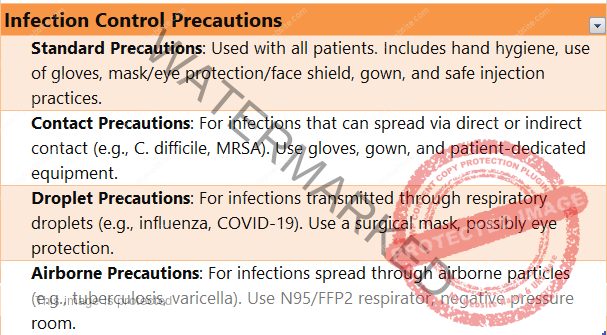
Infection Control Precautions
Infection control precautions are measures designed to prevent the spread of infectious diseases within healthcare settings and the broader community. These precautions are critical for protecting patients, healthcare workers, and visitors from potential infection.
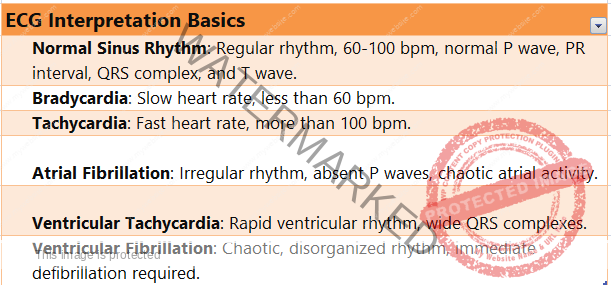
ECG Interpretation Basics
Electrocardiogram (ECG or EKG) interpretation is a fundamental skill in cardiology and emergency medicine, providing valuable information about heart function, rhythm, and structure.
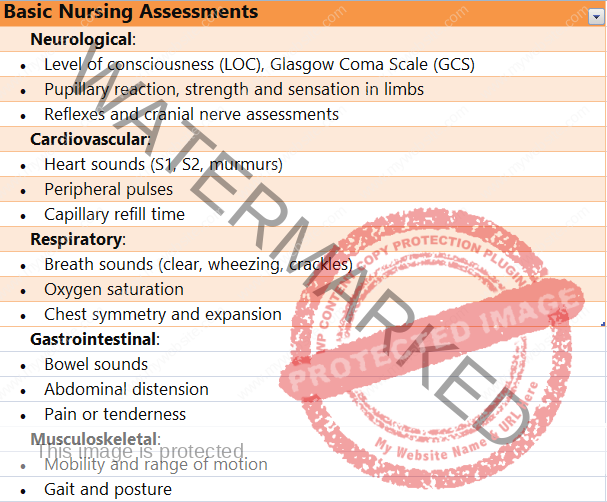
Basic Nursing Assessments
Nursing assessments are essential components of patient care, allowing nurses to evaluate a patient’s health status, identify potential problems, and develop appropriate care plans. Basic nursing assessments encompass a range of physical, emotional, and social evaluations.
General Components of Nursing Assessments
Nursing assessments typically include the following components:
1. Patient History
- Medical History: Previous illnesses, surgeries, allergies, and chronic conditions.
- Medications: Current medications, including prescriptions, over-the-counter drugs, and supplements.
- Family History: History of diseases or conditions that may have a genetic component.
- Social History: Lifestyle factors, such as smoking, alcohol use, drug use, occupation, and living conditions.
2. Physical Assessment
Physical assessments involve a systematic examination of the body, often following the “head-to-toe” approach.
- Vital Signs: Temperature, heart rate, respiratory rate, blood pressure, and oxygen saturation.
- General Appearance: Overall presentation, level of consciousness, and signs of distress.
- Skin: Color, texture, moisture, turgor, presence of rashes, or lesions.
- Head and Neck: Cranial nerve assessment, inspection of eyes, ears, nose, mouth, and neck for abnormalities.
- Chest: Respiratory assessment (e.g., breath sounds, rate, depth, and pattern) and cardiovascular assessment (e.g., heart sounds, murmurs, and rhythm).
- Abdomen: Inspection, auscultation, palpation, and percussion for tenderness, distension, or abnormal masses.
- Musculoskeletal: Assessment of strength, range of motion, and presence of swelling or deformities.
- Neurological: Level of consciousness, reflexes, sensation, coordination, and gait.
- Genitourinary: Inspection for signs of infection, urinary retention, or other abnormalities.
3. Pain Assessment
- Pain Level: Using a pain scale (e.g., numeric rating, Wong-Baker FACES), assess the intensity of pain.
- Pain Location: Identify where the pain is located and whether it radiates.
- Pain Quality: Describe the type of pain (e.g., sharp, dull, throbbing).
- Pain Timing: Determine when the pain occurs and its duration.
4. Psychosocial Assessment
- Emotional Status: Assess for signs of depression, anxiety, or stress.
- Social Support: Evaluate the patient’s support system, including family, friends, and caregivers.
- Spiritual/Religious Beliefs: Understand how these beliefs may impact care and decision-making.
- Cultural Considerations: Be aware of cultural factors that might affect communication and healthcare preferences.
5. Nutrition and Hydration
- Dietary Habits: Assess the patient’s typical diet and fluid intake.
- Weight and Body Mass Index (BMI): Evaluate for significant changes in weight or nutritional imbalances.
6. Functional Assessment
- Activities of Daily Living (ADLs): Determine the patient’s ability to perform basic tasks (e.g., bathing, dressing, eating).
- Instrumental Activities of Daily Living (IADLs): Evaluate tasks like cooking, shopping, and managing medications.
- Mobility: Assess the patient’s ability to move, walk, and transfer.
Techniques and Tools for Nursing Assessments
- Observation: Using visual and auditory cues to identify signs of health problems.
- Auscultation: Listening to internal body sounds using a stethoscope.
- Palpation: Feeling body parts to detect abnormalities in texture, temperature, or tenderness.
- Percussion: Tapping on body parts to detect changes in density or fluid accumulation.
- Documentation: Accurate recording of assessment findings in the patient’s medical record.
Importance of Nursing Assessments
- Early Detection: Identifying health issues early for timely intervention.
- Developing Care Plans: Creating individualized care plans based on assessment findings.
- Communication and Collaboration: Facilitating communication among healthcare team members to ensure coordinated care.
- Patient Education: Educating patients and families about their health and care plans.