Ultimate Guide to prepare Nursing Care Plan
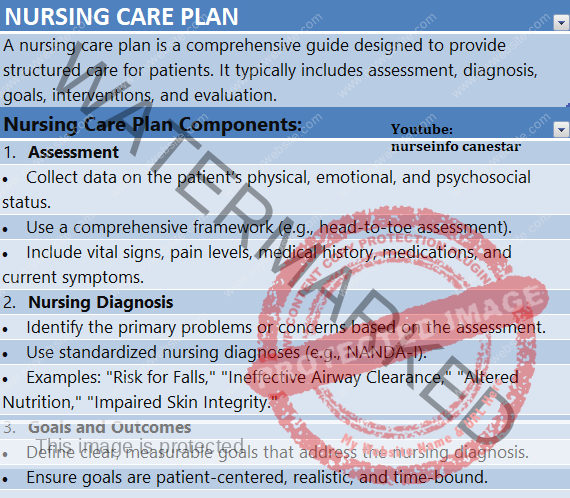
NURSING CARE PLAN
A nursing care plan is a comprehensive guide designed to provide structured care for patients. It typically includes assessment, diagnosis, goals, interventions, and evaluation.
Nursing Care Plan Components:
- Assessment
• Collect data on the patient’s physical, emotional, and psychosocial status.
• Use a comprehensive framework (e.g., head-to-toe assessment).
• Include vital signs, pain levels, medical history, medications, and current symptoms. - Nursing Diagnosis
• Identify the primary problems or concerns based on the assessment.
• Use standardized nursing diagnoses (e.g., NANDA-I).
• Examples: “Risk for Falls,” “Ineffective Airway Clearance,” “Altered Nutrition,” “Impaired Skin Integrity.” - Goals and Outcomes
• Define clear, measurable goals that address the nursing diagnosis.
• Ensure goals are patient-centered, realistic, and time-bound.
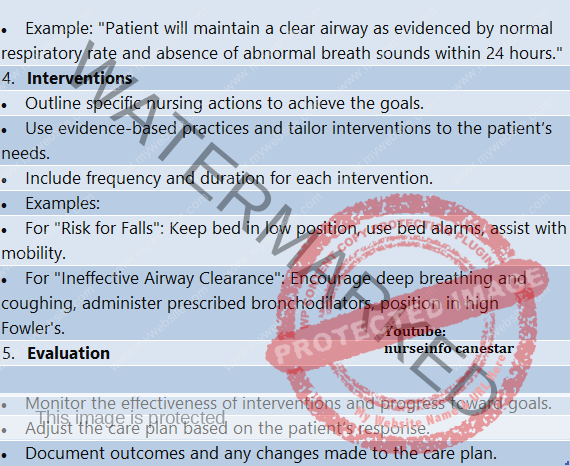
• Example: “Patient will maintain a clear airway as evidenced by normal respiratory rate and absence of abnormal breath sounds within 24 hours.” - Interventions
• Outline specific nursing actions to achieve the goals.
• Use evidence-based practices and tailor interventions to the patient’s needs.
• Include frequency and duration for each intervention.
• Examples:
• For “Risk for Falls”: Keep bed in low position, use bed alarms, assist with mobility.
• For “Ineffective Airway Clearance”: Encourage deep breathing and coughing, administer prescribed bronchodilators, position in high Fowler’s. - Evaluation
• Monitor the effectiveness of interventions and progress toward goals.
• Adjust the care plan based on the patient’s response.
• Document outcomes and any changes made to the care plan.
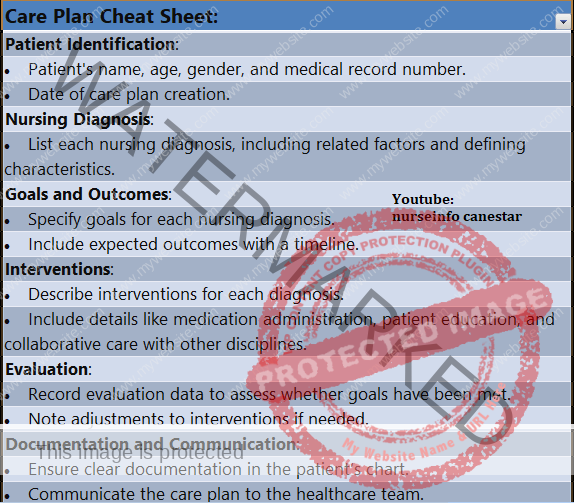
Care Plan Cheat Sheet:
• Patient Identification:
• Patient’s name, age, gender, and medical record number.
• Date of care plan creation.
• Nursing Diagnosis:
• List each nursing diagnosis, including related factors and defining characteristics.
• Goals and Outcomes:
• Specify goals for each nursing diagnosis.
• Include expected outcomes with a timeline.
• Interventions:
• Describe interventions for each diagnosis.
• Include details like medication administration, patient education, and collaborative care with other disciplines.
• Evaluation:
• Record evaluation data to assess whether goals have been met.
• Note adjustments to interventions if needed.
• Documentation and Communication:
• Ensure clear documentation in the patient’s chart.
• Communicate the care plan to the healthcare team.
• Provide a report during shift changes or team meetings.
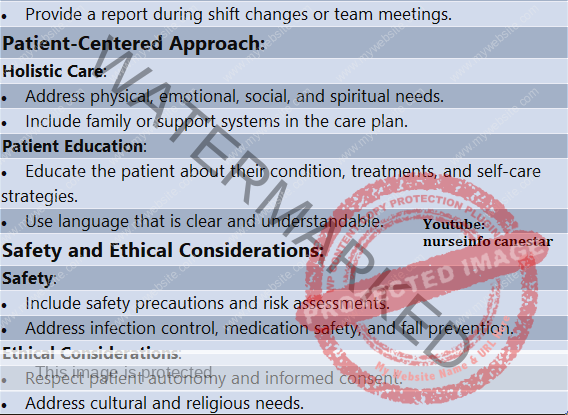
Patient-Centered Approach:
• Holistic Care:
• Address physical, emotional, social, and spiritual needs.
• Include family or support systems in the care plan.
• Patient Education:
• Educate the patient about their condition, treatments, and self-care strategies.
• Use language that is clear and understandable.
Safety and Ethical Considerations:
• Safety:
• Include safety precautions and risk assessments.
• Address infection control, medication safety, and fall prevention.
• Ethical Considerations:
• Respect patient autonomy and informed consent.
• Address cultural and religious needs.