UNCONSCIOUS CLIENTS – NURSING CARE PLAN
NURSING CARE PLAN
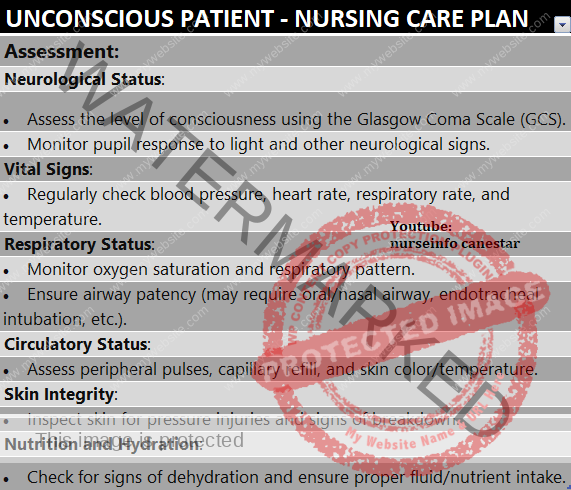
1. Ineffective airway clearance R/T upper airway obstruction by tongue and soft tissues, inability to clear respiratory secretions as evidenced by unclear lung sounds, unequal lung expansion, noisy respiration, presence of stridor, cyanosis, or pallor.
Client Expected Outcome
The client maintains patent airway as evidenced by clear lung sounds, equal lung expansion and absence of stridor, cyanosis and pallor.
Nursing Interventions
– Assess respiratory rate pattern, lung sounds, lung expansion, signs of tissue hypoxia, cyanosis, pallor; presence of airway secretions; occlusion of oropharynx by epiglottis or tongue; aspiration of vomitus or oral secretions.
Rationale: provides data for planning care.
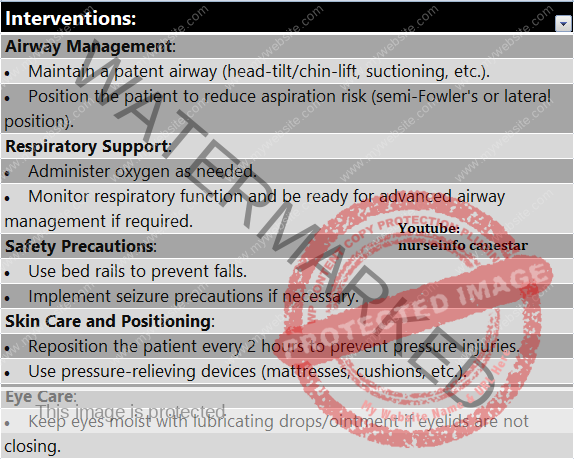
– Elevate had of bed to 30 degree angle or place client in lateral or semiprone position.
Rationale: head elevation prevents aspiration. Lateral position permits the jaw and tongue to fail forward, thus promoting drainage of secretions.
– Insert oral airway (if tongue is paralyzed or is obstructing the airway).
Rationale: prevents obstruction of airway; obstructed airway leads to cerebral hypoxia which increases ICP.
– Suction airway intermittently.
Rationale: in the absence of cough and swallowing reflexes, secretions rapidly accumulate in the posterior pharynx and upper trachea and can lead to aspiration. Intermittent suctioning prevent this.
– Administer humidified oxygen to the airway before and after suctioning.
Rationale: prevents hypoxia which may be caused by sucking out of air while suctioning.
– Initiate chest physiotherapy and postural drainage (unless contraindicated)
Rationale: promotes pulmonary hygiene
– Prepare for endotracheal intubation or tracheostomy
Rationale: allows efficient removal of tracheobronchial secretions and protects the airway from aspiration.
– Connect the client to mechanical ventilator as needed.
Rationale: helps maintaining oxygenation when spontaneous respiration is not possible.
– Increase amount of fluids administered at least 2.5 litre per day.
Rationale: loosens airway secretions promoting easy removal.
– Auscultate chest at least every 8 hours.
Rationale: helps detect adventitious breath sounds or absent breath sounds.
– Monitor ABG measurements.
Rationale: help detect complications of respiratory problems at the earliest.
2. Ineffective cerebral tissue perfusion related to effects of increased ICP as evidenced by papilloedema, Cushing’s traid, vomiting.
Client Expected Outcome
The client maintains optimum cerebral perfusion as evidenced by absence of signs of increased ICP (papilloedema, projectile vomiting, Cushing’s triad, pupillary changes).
Plan of Action
– Assess signs of increased ICP, cerebral edema.
Rationale: provides baseline data.
– Maintain head of the bed elevated to 30 degree angle.
Rationale: promotes venous return through jugular veins thus preventing cerebral oedema.
– Maintain head and neck aligned.
Rationale: hyperextension, rotation, or hyperflexion of neck causes decreased venous return which will lead to cerebral edema formation.
– Administer low flow oxygen and maintain oxygen therapy.
Suction airway when needed.
Rationale: These measures prevent hypoxia.
– Monitor ABG values
Rationale: rapidly increasing blood flow to the brain causing cerebral oedema.
– Maintain PaCO2 (normally 35 – 45 mm hg) through hyperventilation.
Rationale: decreased PaCO2 presents vasodilation and thus reduces cerebral blood volume.
– Administer osmotic diuretics e.g., mannitol or corticosteroids: dexamethasone, as prescribed.
Rationale: osmotic diuretics promote venous return, corticosteroid manage inflammatory response. Both these are used to prevent cerebral oedema.
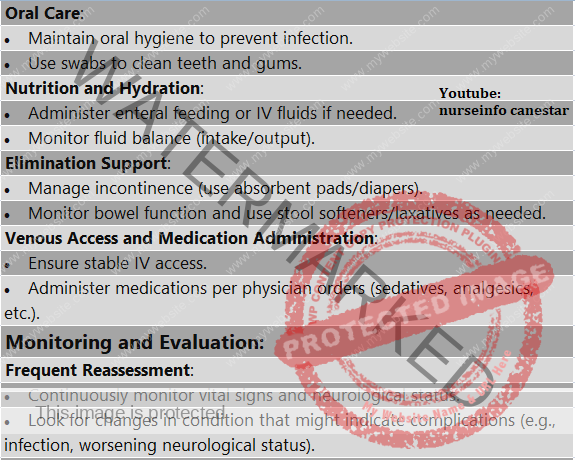
– Administer stool softness as prescribed.
Rationale: soft bowel involvements prevent straining or valsalva maneuver because it will increase intra-abdominal pressure and thereby increasing ICP.
3. Risk for injury related to unconscious state.
Client Expected Outcome
The client remains free of injury
Nursing Interventions
– Assess risk factors for injury – lack of side rails, seizures, loss of corneal blink reflex, invasive lines and equipment, restraints, tight dressings, environmental dressings, environmental irritants, damp bedding or dressings, nail not cut.
Rationale: help obtain data to plan care.
– Keep side rails up and bed in lowest position whenever the client is not receiving direct care.
Rationale: prevent fall and injury.
– Observe seizure precautions for client with history of seizure episodes.
Rationale: seizure without maintaining safety is a common safety hazard among unconscious clients.
– Use padded side rails.
Rationale: prevents injury during seizure activity.
– Keep client’s nail short.
Administer prescribed seizure drugs.
Rationale: helps prevent seizure episodes by maintaining high seizure threshold.
– Use caution when moving the client.
Rationale: unconscious client cannot voice pain.
– Give adequate support to the limbs and head when moving or turning the unconscious client.
Rationale: limbs without tone may dislocate if they are allowed to fall unsupported.
– Always turn the client toward the nurse
Rationale: prevent falls.
– Protect from external sources of heat such as hot water bags.
Rationale: unconscious clients cannot voice pain.
– Release restraints (if used) every 2 hours.
Rationale: helps in providing range of motion exercises; prevents complication of immobility.
– Avoid restraints as far as possible, allow one family member/significant other to be with the client.
Rationale: restraints may worsen the client’s condition if he is confused.
– Keep bed and bedding free of moisture, dust and debris.
Rationale: prevents skin excoriation.
– Avoid over sedation.
Rationale: over sedation alters respirations, which increases ICP and masks changes in level of consciousness.
– Avoid speaking negatively about the client or his condition.
Rationale: the last sense to go is the sense of hearing for psychological integrity.
4. Risk for fluid volume deficit related to inability to ingest fluids, dehydration from osmotic diuretics.
Client Expected Outcome
The client maintains optimum fluid volume state.
Nursing Interventions
– Assess hydration status by examining tissue turgor, mucus membranes, assessing intake and output changes and analyzing laboratory data (BUNS, creatinine, S.Na, S.K, S.Cl, C02)
Rationale: help plan care.
– Hydrate the client with use of IV fluids initially.
Rationale: meet fluid needs rapidly.
– Avoid over hydrating the client with I.V. fluids or blood transfusions.
Rationale: excessive or rapid administration of fluid may lead to cerebral edema and increased ICP.
– Administer fluids slowly.
– Continue fluid administration with use of Ryle’s tube.
Rationale: for long-term fluid administration in unconscious clients.
– Administer corticosteroids and diuretics in suspected cerebral edema.
Rationale: maintain normal volume of fluids.
– Monitor intake and output and urine specific gravity.
Rationale: helps detect abnormality from normal.
– Evaluate peripheral pulses and BP at regular intervals; in severe cases, hemo-dynamic parameters (CVP, PAP, PAWP, CO measurement).
Rationale: these are parameters to measure circulatory adequacy/inadequacy.
5. Ineffective thermoregulation R/T damage to hypothalamic center as evidenced by persistent elevation of body temperature, warm and dry skin, flushed appearance of skin.
Client Expected Outcome
The client maintains thermoregulation as evidenced by normal body temperature.
Plan of Action
– Assess body temperature, look for possible sites of infections (respiratory, CNS, urinary tract, wound, blood, IV sites).
Rationale: provides baseline data. Unconscious clients may have controlled fever because of hypothalamic involvement of infection.
– Monitor temperature frequently or continuously.
Rationale: helps detect changes in temperature and to administer prompt treatment.
– Control persistent elevation of temperature with use of
Antipyretics
Cooling blankets
Adequate fluid intake
Tepid sponge
Cold compress
Well-ventilated room
Rationale: fever increases metabolic demands of brain, decreases circulations and oxygenation resulting in cerebral deteriorations.
– Control shivering in fever with use of
Blankets
Warm environment
Heat applications
By avoiding rapid over-cooling
Rationale: shivering increases metabolic demands ICP.
6. Risk for impaired tissue integrity cornea related to absence of corneal blink reflex, dryness of eyes.
Client Expected Outcome
The client maintains intact corneal tissue integrity as evidenced by moist corneal tissues, absence of corneal ulceration.
Plan of Action
– Assess signs of impaired corneal integrity (corneal drying, irritation, ulceration) look for presence of corneal blink response.
Rationale: data help plan care.
– Protect eyes with an eye shield.
Rationale: if eyes remain open for long periods corneal ulceration will develop.
– Make sure the client’s eye is not rubbing against anything such as bedding or client’s own clothing.
Rationale: in conscious clients, usually blinking and corneal reflexes are absent; can result in injury.
– Inspect the condition of eyes with a flash light at regular intervals.
Rationale: helps detect corneal irritation at the earliest stage.
– Remove contact lenses if worn.
Rationale: prevents corneal dryness and injury.
– Irrigate eyes with sterile saline or prescribed solution as ordered.
Rationale: remove discharge and debris, prevents inflammation.
– Instill prescribed ophthalmic ointment in each eye.
Rationale: prevents glazing and corneal ulceration.
– Instill artificial tears as prescribed.
Rationale: keep eyes moist thereby preventing corneal dryness.
– Apply eye patches when indicated.
Rationale: ensures that eyes remain closed under patch.
– Prepare for temporary tarsorrhaphy (suturing of eyelids in closed position).
Rationale: keeps eyes closed in case unconscious state is prolonged.
7. Altered oral mucous membrane related to mouth breathing, absence of pharyngeal reflex, inability to ingest fluid as evidenced by dryness, inflammation crusting and halitosis.
Client Expected Outcome
The client maintains intact oral mucous membrane as evidenced by absence of dryness, inflammation, crusting and halitosis and presence of pink, moist mucous membranes.
Plan of Action
– Assess oral mucous membrane for dryness, cracks, encrustation, and signs of inflammation.
Rationale: helps plan appropriate care.
Parotitis is common in unconscious client whose mouth is unclean.
– Inspect mouth every 8 hours using flashlight and tongue depressor; if dentures present, remove them and then inspect.
Rationale: helps detect problems in earlier stage.
– Cleanse and rinse mouth carefully with appropriate solution every 2 to 4 hours.
Rationale: keep mucous membranes clean, moist and free of inflammation (e.g., parotitis).
– Apply thin coat of petrolatum on lip after oral care.
Rationale: prevents drying, cracking and encrustation.
– Avoid use or lemon or alcohol-containing agents clearing.
Rationale: cause dryness.
– Gently swab nose with wet cotton applicator and apply water-soluble lubricant.
Rationale: remove encrustations from nose and facilitates nose breathing preventing dryness of mouth from mouth breathing.
8. Imbalanced nutrition – less than body requirement, related to inability to eat and swallow as evidenced by weight and other nutritional parameters less than normal
Client Expected Outcome
The client maintains optimum nutrition as evidenced by stable weight, adequate calories for age, height and weight, balanced intake and output, normal Hb, BUN, total lymphocytes, total proteins and serum albumin.
Plan of Action
– Assess nutritional status and requirements Ht-Wt, lab tests, signs of malnutrition dry and loose skin and mucous membrane emaciated appearance.
Rationale: provides baseline data to plan the care.
– Administer fluids intravenously, meeting nutritional requirement, with careful monitoring of fluid intake and output.
Rationale: intravenous administration meets nutritional requirements rapidly; too rapid administration of fluids lead to cerebral oedema formation.
– Administer fluid diet in the form of juice, shake, soup, porridge, water via Ryle’s tube.
Rationale: unconscious client cannot take oral feeds. These feeds meet nutritional requirement. Unconscious clients have increased metabolic needs (immunodeficiency, proteins wasting, lung tissue, catabolism, negative nitrogen state).
– Initiate TPN, if the client cannot tolerate Ryle’s tube feeds (excessive vomiting, regurgitation, decreased peristalsis, absent bowel movement).
Rationale: meets nutritional requirements of coma clients.
– Monitor nutritional parameters (Ht, Wt, lab test, clinical examinations) at regular intervals.
Rationale: help determine nutritional adequacy or inadequacy.
9.Self care deficit (bathing, feeding, grooming, toileting) related to unconscious state as evidenced by unkempt and poorly nourished look, constipation, bed soiling.
Client Expected Outcome
Client’s self care needs are met as evidenced by neat and groomed appearance; nourished look, absence of soiling of bed and constipation.
Plan of Action
– Assess self-care needs; self-care deficits of the client, availability of care given to perform self-care activities.
Rationale: provides baseline data to plan care.
– Perform bed bath daily and as required (upon soiling of bed with stool, urine, sweat or dirt).
Rationale: clean skin prevents bacterial growth. Promotes overall well-being
– Provide oral hygiene 4 hourly.
Rationale: unconscious clients suffer from problems of neglected mouth such as inflammation. Oral and nasal mucosa dryness, halitosis, spread of infection to adjacent structures.
10. Risk for complications – pressure sores, contractures, deep vein thrombosis, hypostatic pneumonia, constipation – related to immobility
Client Expected Outcome
The client remains free of complications associated with immobility
Plan of Action
– Give skin care to pressure prone areas hourly
Rationale: massage increases circulation; skin cleanliness is needed to prevent pressure sore by moisture and excessive dryness.
– Avoid vigorous massage of bony prominences.
Rationale: vigorous massage causes skin excoriation over bony prominences.
– Provide high calorie, high protein, vitamin-rich diet with more amounts of fluids (diet in the form of fluids such as porridge, soup, shake, juice).
Rationale: adequate nutrition and fluid intake keep the skin nourished, thus prevents pressure sore formation.
Contractures and Joint Deformity, Muscle Wasting
– Keep the body in the anatomical position with use of devices like footrest, trochanteric rolls, sand rags, rolled cloth, waterfilled gloves, etc.
Rationale: keeping the body aligned helps prevent joint deformity and contractures.
– Give protein-rich diet.
Rationale: maintain positive nitrogen balance. Keeps muscles straightened.
– Perform range of motion exercises 4 hourly after removing the support devices.
Rationale: passive exercise helps straightened weak muscles; looses spastic muscles; promote joint flexibility and increase overall well-being of the client.
DVT
– Elevate lower extremities above the heart level intermittently for 20 minutes.
Rationale: helps increase venous return, thus preventing thrombus formation.
– Perform passive range of motion exercises to extremities 4 hourly.
Use elastic stockings as required.
Monitor and compare the circumference of both legs at regular intervals.
Rationale: difference in leg circumference indicates DVT.
– Monitor for presence of redness, swelling and increased temperature of legs.
Rationale: the signs of inflammation indicates DVT.
Hypostatic Pneumonia/Aspiration Pneumonia
– Suction the airway at regular intervals.
Rationale: unconscious clients are unable to remove oral and airway secretions.
– Accumulation of secretion leads to pneumonia.
– Change position 2 hourly.
Rationale: prevents pooling of secretions in the lungs thus preventing hypostatic pneumonia.
– Initiate chest physiotherapy and postural drainage unless contra-indicated.
Feed the client in head elevated position.
Rationale: prevent aspiration of oral secretions and content, thereby pneumonia.
– Aspirate Ryle’s tube before feeding.
– Watch for regurgitation and vomiting.
– Keep head turned to one side.
– Give fluids (compatible with output)
Rationale: helps loosen airway secretions facilitating easy removal.
Constipation
– Provide adequate fluids.
Rationale: increased fluids required for softening the faeces.
– Administer stool softness and enema as indicated.
Rationale: helps in easy bowel evacuation.
– Change position 2 hourly.
Rationale: change of position increases the bowel movements.
– Administer commercially available bowel evacuation powders (given in the form of liquid) as ordered.
Rationale: These preparations help form stools and facilitate bowel evacuation.
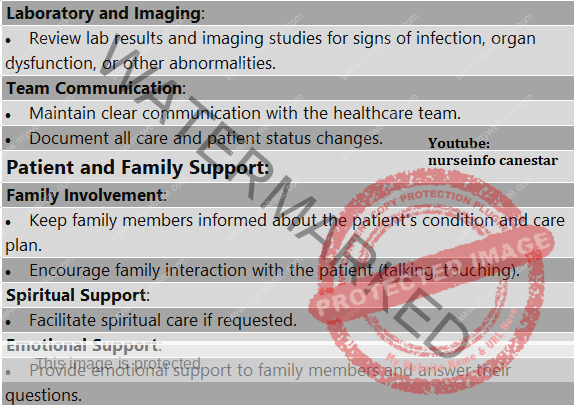
11. Interrupted family process related to chronic illness of a family member as evidenced by anger, grief, non-participation in client care.
Client Expected Outcome
The family demonstrates increased coping as evidences by showing an ability to solve problem, not neglecting the needs of family members.
Plan of Action
– Assess family’s response towards the client’s illness-severe anxiety, denial, anger, remorse, grief, reconciliation-then usual use of coping mechanisms, role of client in the family, communication pattern, social support available, financial status, relationship between family members.
Rationale: provides baseline data which helps to plan care.
– Develop a supportive and trusting relationship with the family or significant others.
Rationale: high establish interpersonal relationship which is the keystone for care.
– Provide information and frequent updates on client’s condition and progress.
Rationale: helps alleviate anxiety and to cope better with client’s condition.
– Involve family in routine care, teach procedures that they can perform at home.
Rationale: a sense of responsibility helps to reduce anxiety; promotes continuity of care.
– Demonstrate and teach methods of sensory stimulation to be used frequently.
Use physical touch and reassuring voice
– Talk in a meaningful way even when client does not seem to respond.
– Orient person periodically to person, place and time.
Rationale: these interventions help family to understand that the client is having internal awareness of what is going on around, through he is not responding to stimuli. This understanding will help them to better cope with client’s condition; and reduce their anxiety to a greater extent and increase their participation in client care.
– Teach family to recognize and report unusual restlessness of the client
Rationale: restlessness may indicate cerebral hypoxia or metabolic imbalance.
– Enlist help of social worker, home health agency or other resources.
Rationale: assist family with such issues as financial concerns, need for medical equipment in home and respite care.